Government Healthcare Insights
MACRA: Accelerating the Shift to Value-Based Care
September 28, 2017
In a recent blog post by my colleague, we explored how Population Health Management capabilities are becoming increasingly important in the era of value-based care. Today, we continue on the theme of value-based care but pivot our focus to recent legislation and Centers for Medicare & Medicaid Services (CMS) initiatives that are dramatically accelerating the shift to value.
The Medicare Access and CHIP Reauthorization Act (MACRA), which was passed as legislation in 2015, is the largest change in a generation to Medicare physician reimbursement. MACRA places most providers that receive Medicare fee-for-service (FFS) reimbursement, regardless of care setting or specialty, on the road toward value-based arrangements:
- MACRA repealed the sustainable growth rate, which means the 2015 Medicare fee schedule is frozen. Therefore, in order for providers to receive Medicare reimbursement increases (or even keep pace with inflation), they must participate and succeed in value-based arrangements.
- MACRA also established the Quality Payment Program (QPP), which requires providers with Medicare FFS reimbursement to participate in one of three new payment models:
- Merit-Based Incentive Payment System (MIPS) – the default reimbursement model under QPP.
- MIPS APM – an alternative that allows providers to participate in MIPS with reduced reporting requirements and preferred scoring. MSSP Track 1 ACOs are the primary model under MIPS APM.
- Qualifying Alternative Payment Model (QAPM) – value-based reimbursement models with downside risk (e.g., Next Gen ACOs, MSSP Track 2 and 3 ACOs, CPC+, ESRD, and Oncology Care Model).
The majority of providers are not ready to successfully participate in downside risk models, making QAPM models a poor choice for many providers at this time. Therefore, most providers will participate in MIPS or MIPS APMs. Under these two models, providers submit quality and cost data to CMS and receive a MIPS score that places each provider on a bell curve that shifts payments from low-performing providers to high-performing providers:
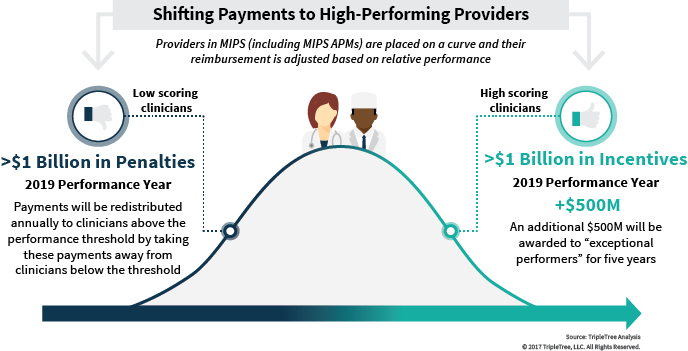
These payment adjustments start in 2019 (based on 2017 performance), and will grow in materiality each year until 2022+ when providers face up to a 9% positive or negative adjustment, depending on where they land on the bell curve. Providers on the left side of the bell curve will clearly suffer. In addition, with the sustainable growth rate repealed under MACRA, being an average provider in the middle of the bell curve is also a losing proposition due to inflation eroding the value of the reimbursement. The only way for providers to receive Medicare FFS reimbursement increases in the future is to be on the right side of the reimbursement bell curve.
This is where MIPS APMs (MSSP Track 1 ACOs) become an important part of the story. CMS’s stated goal is to move a majority of providers into alternative payment models (APMs) with downside risk over time. For most providers, an approach with limited to no downside is the path to success in the shift to value, and CMS is incentivizing providers to do just that through Track 1 ACOs:
- In a Track 1 ACO, providers are incentivized through shared savings bonuses to build the IT, analytics, governance, and clinical infrastructure and capabilities required to succeed in value-based care without facing any downside risk.
- As such, Track 1 ACOs represent an ideal initial step for providers in the shift to value.
- Recognizing this, CMS structured MIPS to give providers in Track 1 ACOs reduced reporting requirements and preferred scoring, putting providers in Track 1 ACOs at a significant advantage to achieve MIPS scores that will place them on the right side of the reimbursement bell curve. The exact same physician practice earns a much higher MIPS score when reporting within a Track 1 ACO versus default MIPS.
From TripleTree’s perspective, we believe MACRA is accelerating the market’s shift to value, and that Track 1 ACOs will play a big part in this acceleration. Providers will be looking for technology and services solutions that can help enable this shift, creating exciting opportunities for innovation, disruption, and investment. We will continue to closely monitor the impact of MACRA and Track 1 ACOs on the shift to value and would love to know what you think.
