Care Management
Medicaid in the “New Normal”
May 21, 2020
In this third installment of our blog series we explore the implications of COVID-19 on Medicaid programs, including accelerated adoption of virtual health capabilities, based on perspectives derived from conversations with business leaders and innovators over the past several weeks.
With the number of people now unemployed approaching 1 out of every 4 working Americans, and the number of people filing initial unemployment claims reaching nearly 39 million people since mid-March, the economic toll of COVID-19 is starting to unfold. While the depth of the economic downturn and shape of our eventual recovery are topics of continued debate, it is not unreasonable to assume that Medicaid enrollment will increase over the coming weeks and months. A recent HMA study estimated that Medicaid enrollment could increase by 11-23 million members as a result of COVID-19. Further, Centene, the country’s largest provider of managed Medicaid and ACA plans, recently increased its 2020 revenue guidance by approximately $6 billion, largely reflecting expected increases in enrollment. Quickly expanding Medicaid rolls will likely coincide with a period of slumping state-level revenue, creating significant budgetary pressures that are unlikely to be filled without additional federal support beyond temporary cost-sharing increases included in the initial CARES Act.
Medicaid populations are among the most adversely impacted by the new realities setting in across the healthcare system and economy. Mounting job losses can be expected to exacerbate already-prevalent social factors like food insecurity and access to affordable housing – which together represent nearly 70% of low-income Medicaid household expenditures – that have a well-documented relationship with poorer physical health. For example, Medicaid beneficiaries under 65 are 2x more likely to be diabetic as compared to individuals with private insurance, and low-income Americans report that multiple chronic conditions limit activities of daily life at a 2-3x greater rate than people with higher incomes. Complicating matters further, COVID-19 has had a chilling effect on preventative and chronic care utilization as, according to a recent Revel Health / Harris survey, 66% of Americans have postponed or cancelled healthcare visits during the pandemic (Revel Health is a TT Capital Partners portfolio company). These social and physical complexities require active management to improve physical health outcomes and avoid unnecessary utilization.
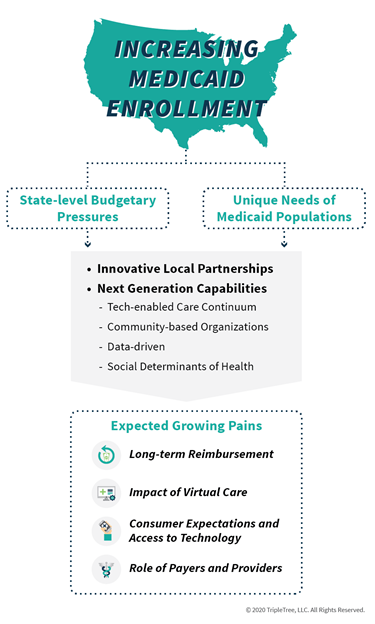
Given the confluence of factors described above, states across the country – especially those that expanded Medicaid – will likely negotiate with managed care organizations (MCOs) to adopt cost containment methods used in previous downturns at a time when safety-net providers are under extreme financial strain themselves. While these measures, including caps on provider payments and drug formulary restrictions, are helpful from a cost perspective, they do not address structural access, cost, and quality challenges. As such, we believe states will begin looking for MCOs to accelerate adoption of capabilities that increase access to higher quality and lower-cost care. As we have recently written, COVID-19 has spurred a new era of virtual health, and Medicaid MCOs are part of this acceleration. AHIP published a report highlighting innovations being deployed, which include improving access via telehealth coverage. In addition, CMS recently released a toolkit for states to consult in adopting expanded telehealth coverage for Medicaid and CHIP. We are encouraged by these developments as leveraging virtual care for Medicaid members can expand access to care while being be both scalable and cost-effective. We have observed examples of MCOs, states, and even providers taking action to ensure Medicaid populations have access to virtual care.
- CareFirst Community Health Plan (f/k/a Trusted Health Plan) has deployed an integrated local strategy that supports its Federally Qualified Health Center (FQHC) partners, encourages the use of telehealth to improve access to care, supports broader behavioral health and engages community-based organizations (CBOs) to support the unique needs of its Medicaid members in the Washington D.C.
- Centene recently teamed up with the National Association of Community Health Centers (NACHC) to help FQHCs adopt telehealth. Interestingly, the effort will bring FQHCs together to pursue a national telehealth strategy for Medicaid programs.
- The State of Massachusetts has responded by partnering with Doctor on Demand to provide free visits for COVID-19 related issues to the state’s 1.8 million Medicaid enrollees. Further, the state’s Medicaid and Children’s Health Insurance Program (CHIP) administrator, MassHealth, is working with Maven to provide telehealth access for individuals experiencing COVID-19 symptoms.
- Louisiana-based health system Oschner is putting a portion of its $1 million FCC COVID-19 telehealth grant to work by distributing more than 1,000 TytoCare at-home telehealth kits to Medicaid and other at-risk populations.
Clearly, healthcare is now being accessed in new ways as the result of COVID-19. With such a profound shift toward digital distribution channels, next-generation healthcare companies that can deliver at scale while addressing the unique needs of Medicaid populations have a significant opportunity to enable quality care in this unprecedented environment. Below are a few of examples of companies we have seen in the marketplace that are well-positioned in the current Medicaid environment and beyond.
- AuntBertha’s online social care network enables non-profits, social care providers, and health care entities to find and coordinate the delivery of social services in their communities.
- Cityblock delivers community-based primary care, behavioral health care and social services to patients at local “neighborhood hubs”, the patient’s home, or virtually.
- Healthify deploys a platform that connects health care organizations to a curated list of local community resources, with the ability to coordinate and track referrals for at-risk populations to measure the impact of social interventions.
- MedZed is a provider of in-home primary and palliative care plus social support for complex Medicaid and Medicare Advantage members through a telehealth-based solution in which in-home nurses are augmented by virtual complex care providers. (MedZed is a TT Capital Partners portfolio company)
- NowPow provides a community resource referral and analytics platform for health care organizations and members to find and access resources based on a member’s zip code.
- Signify Health, through its Signify Community business, provides a platform that coordinates an integrated network of community resources for health plan members facing social determinants. (Signify Health is a TT Capital Partners portfolio company)
- Unite Us provides technology for health care entities to create and manage networks of community-based organizations to address social barriers.
Although COVID-19 is creating a myriad of painful issues, including unprecedented job and economic losses, stretched state budgets, consumer fear, and many more, it has also proven an effective catalyst for all market participants to experiment with new ways to deliver and experience care. As we think ahead toward the transition from crisis to “new normal”, we anticipate natural growing pains as consumers, payers, providers, and regulators look to optimize and normalize the accelerated adoption of innovative solutions. Important future considerations will no doubt include:
- Long-term virtual care reimbursement strategies and long-term sustainable utilization
- The impact of virtual care capabilities on existing health plan preferred network relationships
- The appropriate balance between virtual and in-person care
- Consumer expectations and access to technology to utilize virtual health
- Role of the payer and provider in an evolving ecosystem
While the catalyst (COVID-19) is unfortunate, we look forward to seeing how the industry continues to respond and adapt as it addresses the realities of the pandemic and support state Medicaid programs across the country. Thank you for reading and stay healthy!
Related Blogs:
AUTHOR(S)
TAGS
Community Health, Medicaid, Social Determinants of Health, virtual health

