Care Management
The Evolution of Community-Based Healthcare
October 15, 2020
The concept of community-based care is not a novel one. We’ve heard it for years: healthcare is local. More recently however, constituents across the healthcare system are driving focus on what that truly means. The concept of “total person care” that surrounds an individual through his or her care journey – from finding the optimal clinical setting (at a health system, in the community, in the home), to mental health, to addressing the broader social determinants of health needs (transportation, food, housing, and more) is gaining traction. Now factor in the growing Medicaid rolls, an aging population, and budgetary pressures at both the state and federal level, and we have the perfect catalyst for industry innovation – and the evolution of community-based healthcare.
Core to this evolution is the promise of the elusive “Triple Aim”: a more convenient and optimal healthcare experience that costs less and delivers improved health outcomes. As payers, care providers, and consumers drive industry transformation, a large portion of that effort is focused on pulling from the technology innovation, convenience, and engagement efforts that have been pioneered in other industries but have largely fallen behind in healthcare. With this convergence of a more demanding healthcare consumer, the need to control spiraling healthcare costs, and the growth in chronic patients that require more hands-on, personalized care that looks beyond the clinical profile, the healthcare industry will need to continue optimizing new models of care that create a more integrated and aligned healthcare delivery continuum.
Responding to Consumers with Higher Expectations
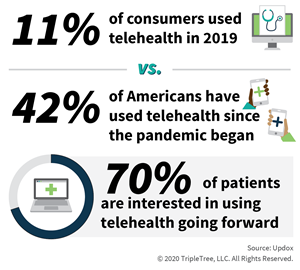
Providers and healthcare organizations can do everything in their power to drive ease and access to care for their patients, but the reality is people are hard to reach, and not everyone considers a doctor visit as a regular part of life. In fact, the COVID-19 pandemic has reignited the push for more convenient and safe care, which demonstrates how consumers are expecting more and more from the healthcare system. This evolution is being addressed across multiple channels, from physically putting access to preventative care into the community or the home, to responding to the consumer’s willingness to connect with providers via telemedicine, including digital messaging, video visits, and telehealth. To enable this convenience, providers are developing models that take care to members, increasing the likelihood of care being delivered. Healthcare organizations have found that engaging with a member in their community increases the ability to drive other initiatives for plans, including gap closure, information gathering, risk assessments, and more. Ultimately, considering convenience in member offerings is a ‘win-win-win’ for providers, plans, and members. By providing the experiences that members are accustomed to in other industries, patient outcomes will be enhanced at lower costs for plans, providers, and patients.
Addressing the Total Person and the Social Determinants of Health (SDoH)
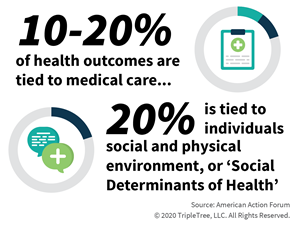
Part of what makes community-based care so critical is the fact that there are so many factors that impact the health of a patient beyond their clinical profile. In fact, recent estimates found that only 10 – 20% of health outcomes are tied to medical care, while 20% is tied to that individuals social and physical environment, or ‘Social Determinants of Health’. The entire healthcare ‘experience’ is cohesive; if a patient doesn’t have access to appropriate nutrition, or a home environment conducive to recovery, or the ability to receive appropriate drugs and follow-up care, it is inconceivable that the system can drive optimal outcomes at efficient costs. Communication across a member’s lifecycle is also critical, keeping them and their family caregivers an engaged member of the care team from the health system into the home, and everywhere in between. To drive this connection, and bridge between the clinical and social-sides of healthcare, healthcare constituents require advanced analytics to assess performance, trends, and key areas for improvement, ultimately identifying the right care in the right setting for the right patient.
Controlling the Cost of Quality Care
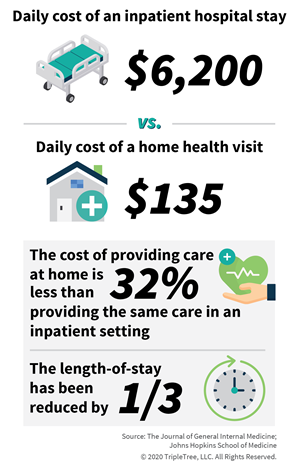
While offering the convenience of community-based care has a ‘consumer-focused’ element to it, the reality is that when delivered correctly it also brings significant cost benefits to the healthcare system as well. Studies have repeatedly found that the cost-of-care in the home in significantly less expensive than acute care settings. In fact, the Journal of General Internal Medicine found that average daily cost of an inpatient hospital stay at $6,200 versus the average cost of a home health visit at $135. Similarly, the Johns Hopkins School of Medicine has found the cost of providing care at home 32% less than providing the same care in an inpatient setting, as well as reducing the length-of-stay by one-third. Cost savings across the continuum of care is a long-term initiative and won’t be solved overnight, driven through active participation and cross-setting care delivery, rather than one-time doctor visits and hospital admissions. Managing patients once they leave the health system can be an incredible burden without the appropriate engagement and care plans in place, and the ability to control what resources and care patients have access to following a medical event, including drug adherence and access to follow-up visits, is mission-critical and can’t be achieved simply through traditional care delivery.
Conclusion
The healthcare industry is poised for change and innovation, as the traditional models for patient care are being reinvented through a focus on access, convenience, affordability and a commitment to total person care. Further accelerated by the pandemic, tech-enabled capabilities and innovative models of consumer engagement are more accessible and integral to comprehensive care, changing the mechanisms through which care is delivered and measured. By driving deeper levels of care in the community and outside of acute-settings, health plans and providers are able to optimize outcomes and costs, all while reshaping consumer expectations of the future healthcare world.
Don’t forget to join us at our next Market Insights LIVE session to hear more about the evolution of community-based healthcare.

It Takes a Village: Evolving Models of Community-Based Care
Tuesday, October 20 | 10:00 AM CT
Click Here to Register
AUTHOR(S)
TAGS
Community-Based Care, Home Health, Market Insights LIVE, SDOH, Social Determinants of Health, Telehealth



